Physical Exam Template Soap Note
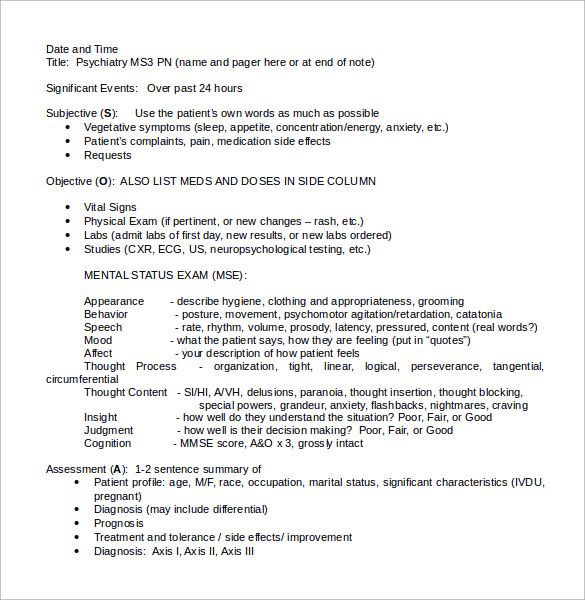
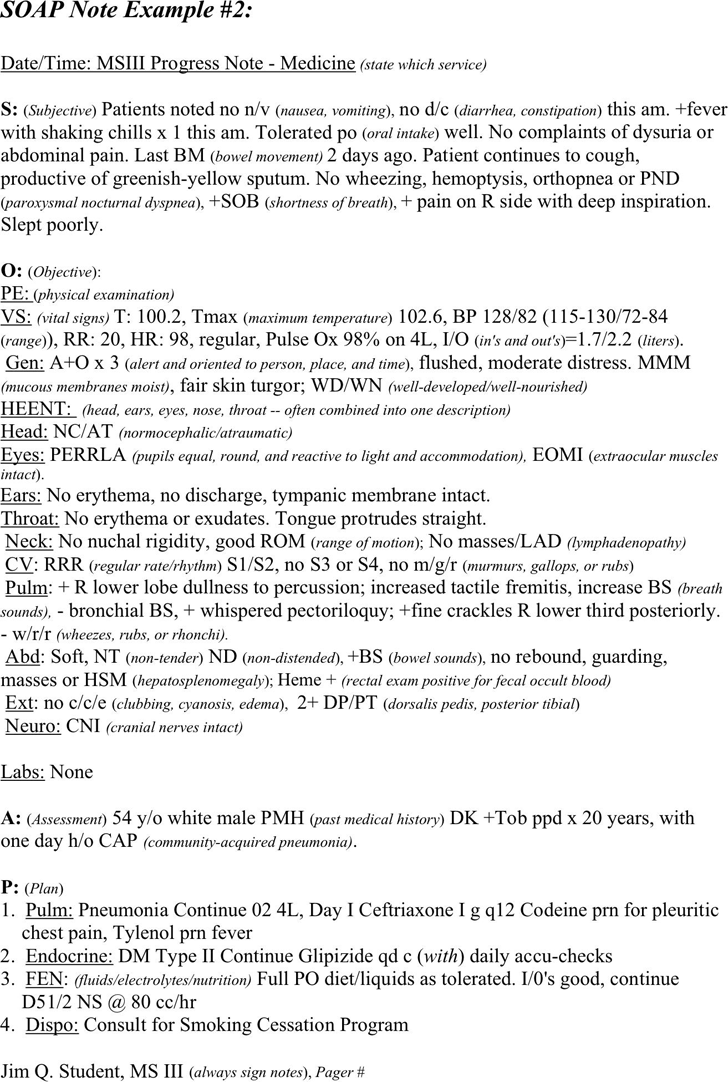
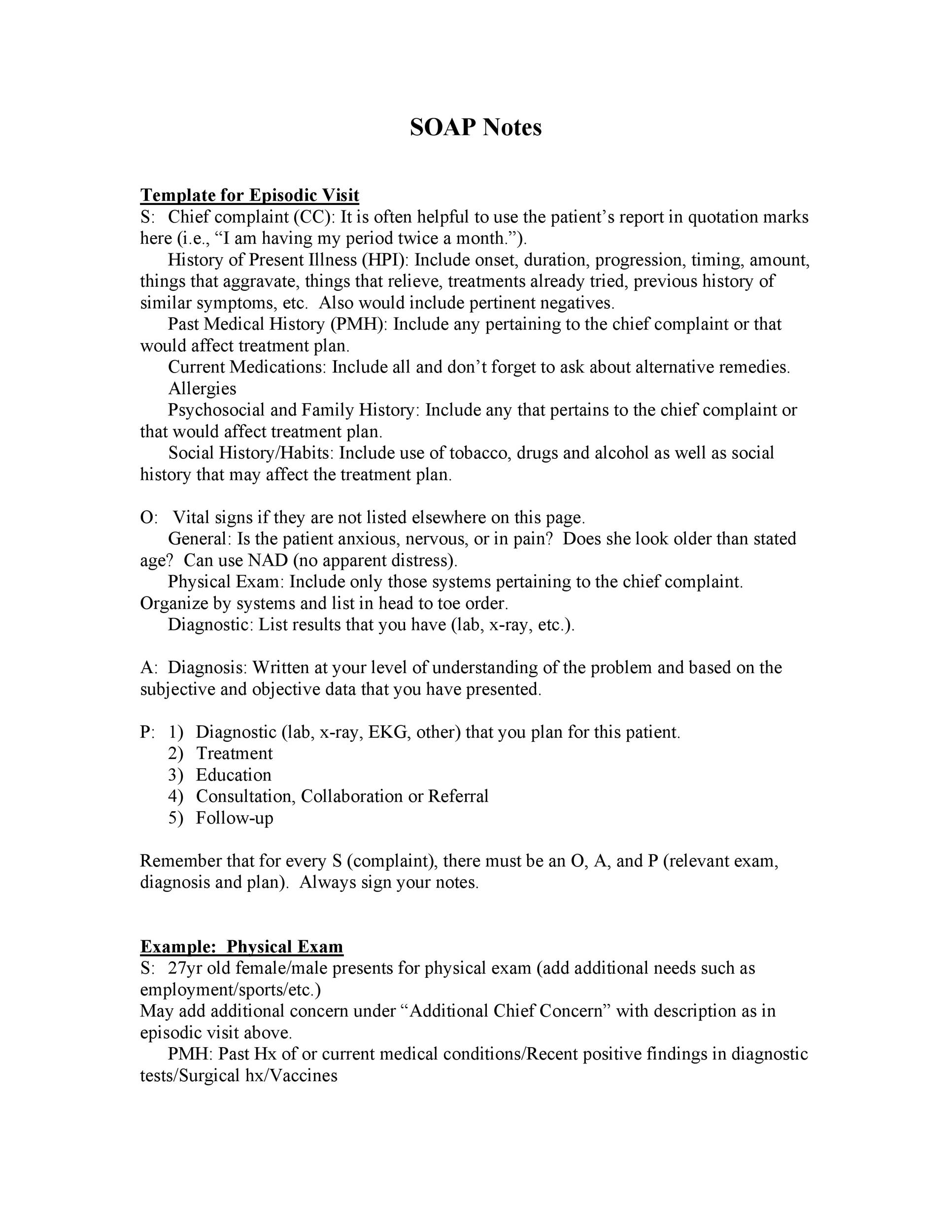
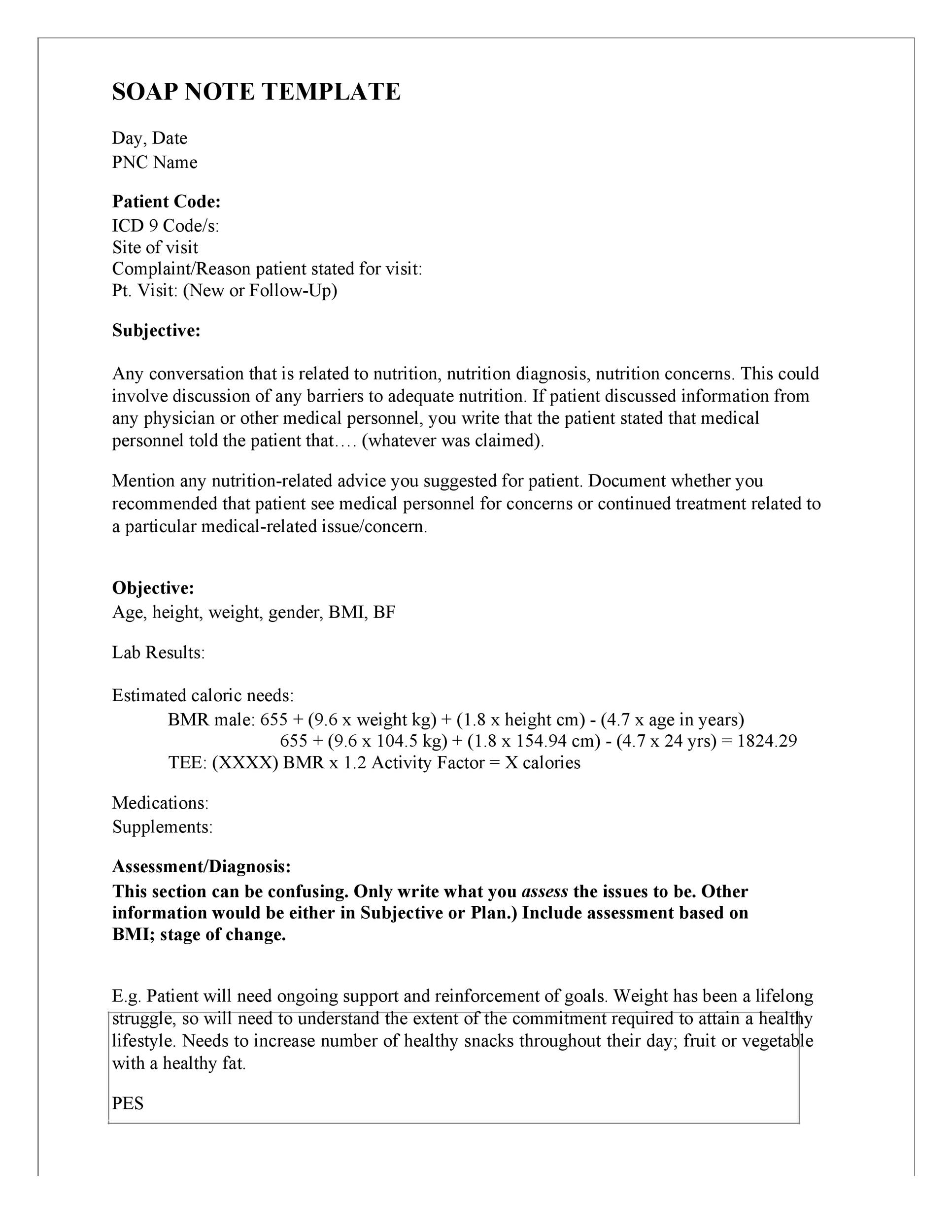
Physical Exam Template Soap Note - Web nurses can use this soap note template to collect patient’s information for admission purposes. Web finally (disclaimer alert!), this post is not an exhaustive documentation reference. Web (listed are the components of the all normal physical exam) a: Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. This is a pleasant, cooperative,. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Web physical therapy soap note example (sample) to help you visualize what a completed soap note will look like using. Web “how are you today?” “how have you been since the last time i reviewed you?” “have you currently got any troublesome symptoms?” “how is your nausea?” if. Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for. Here are the soap note templates that you. Web finally (disclaimer alert!), this post is not an exhaustive documentation reference. Web health professionals must have an accurate record of their patients. Web template for physical therapy soap notes here is a template you can use to guide your soap notes: Web physical therapy soap note example (sample) to help you visualize what a completed soap note will look. Approximately 560 views in the last month. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of. Web physical exam normal medical template transcription samples. Web soap notes vivek podder; Web template for physical therapy soap notes here is a template you can use to guide your soap notes: Web general adult physical exams. Here are the soap note templates that you. Web physical exam normal medical template transcription samples. This is a pleasant, cooperative,. Web physical therapy soap note example (sample) to help you visualize what a completed soap note will look like using. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Author information and affiliations last update: The soap note template is a documentation method used by medical practitioners to assess a. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. The soap note template is a documentation method used by medical practitioners to assess a patient's. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Web a soap note is. Here are the soap note templates that you. Web nurses can use this soap note template to collect patient’s information for admission purposes. Web soap notes vivek podder; Web physical exam normal medical template transcription samples. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. Web finally (disclaimer alert!), this post is not an exhaustive documentation reference. It’s meant to be a practical tool. Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for. Alert and oriented x 3. Web physical exam normal medical template transcription samples. Alert and oriented x 3. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. Web physical exam normal medical template transcription samples. Approximately 560 views in the last month. Web soap notes vivek podder; Here are the soap note templates that you. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. It’s meant to be a practical tool. Alert and oriented. Web (listed are the components of the all normal physical exam) a: Approximately 560 views in the last month. Web soap notes vivek podder; Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many. The soap note template is a documentation method used by medical practitioners to. This is a pleasant, cooperative,. Web general adult physical exams. Web finally (disclaimer alert!), this post is not an exhaustive documentation reference. Web nurses can use this soap note template to collect patient’s information for admission purposes. The soap note template is a documentation method used by medical practitioners to assess a patient's. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of. Approximately 560 views in the last month. Web physical exam normal medical template transcription samples. Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for. Web the soap note (an acronym for subjective, objective, assessment, and plan) is a method of documentation employed by healthcare. It’s meant to be a practical tool. Normal physical exam template |. Web soap notes vivek podder; Web physical therapy soap note example (sample) to help you visualize what a completed soap note will look like using. Web template for physical therapy soap notes here is a template you can use to guide your soap notes: Gastroenterology & hepatology, objective/exam elements. Author information and affiliations last update: Web “how are you today?” “how have you been since the last time i reviewed you?” “have you currently got any troublesome symptoms?” “how is your nausea?” if. Web this veterinary physical exam template is based on the soap template for a veterinary physical exam and evaluation. Here are the soap note templates that you.Physical Exam Soap Note Example
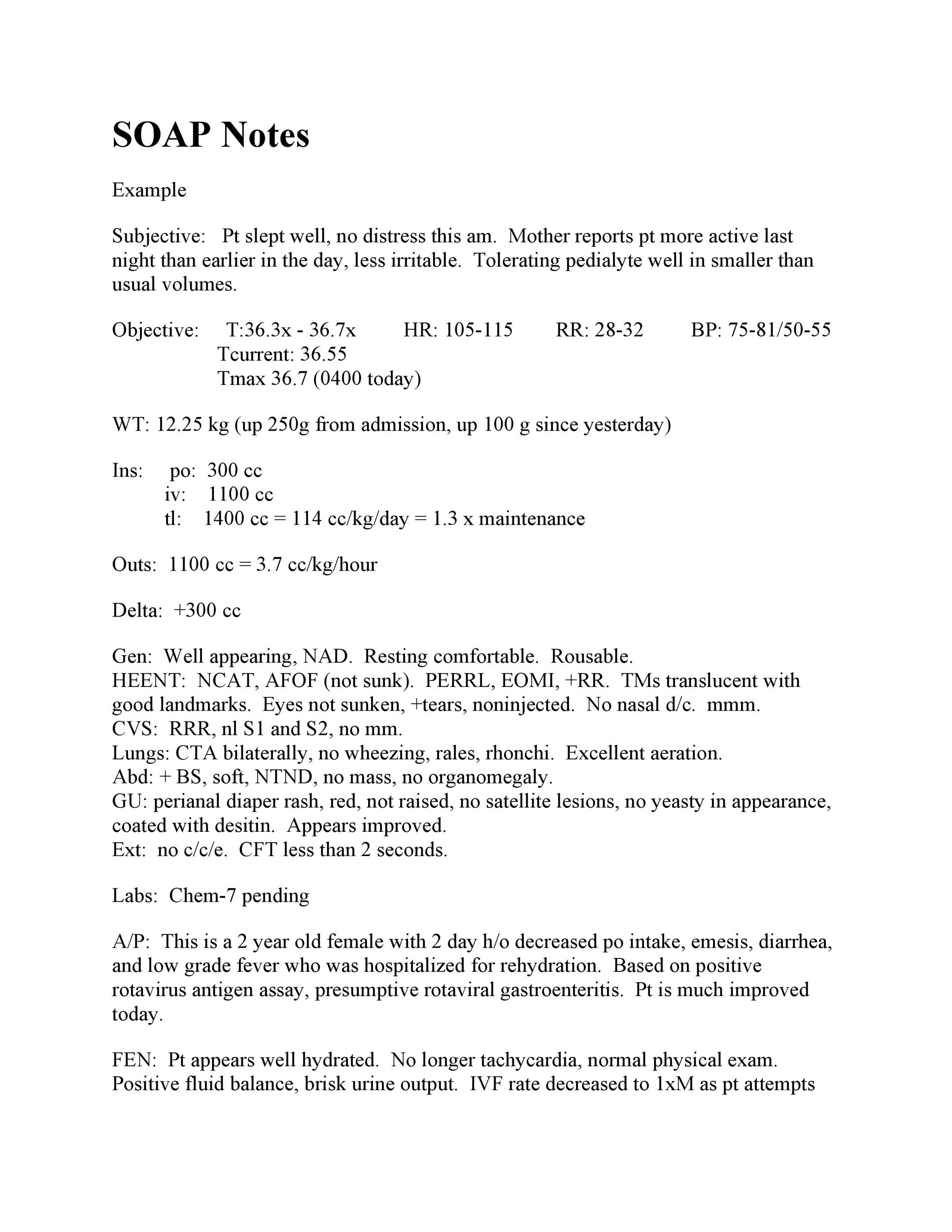
klauuuudia Pediatric Physical Exam Template
Physical Therapist SOAP Notes Example Soap note, Physical therapy
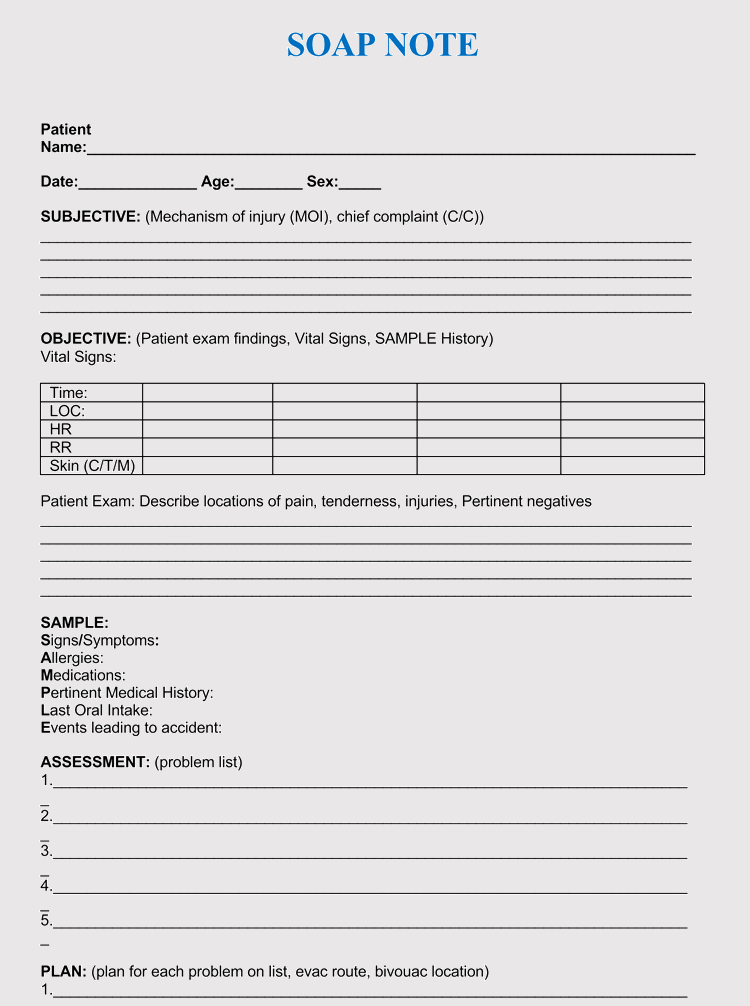
Free SOAP Note Example PDF 102KB 1 Page(s)
klauuuudia Pediatric Physical Exam Template
How to Make Soap Notes Soap note, Soap making, Solution focused therapy
Comprehensive Physical Exam Template Sample Templates
Physical Therapy Soap Note For Stroke Patient United Health Care
Soap Report Template (8) TEMPLATES EXAMPLE TEMPLATES EXAMPLE Soap
SOAP Note PDF Medicine Diseases And Disorders
Related Post: